- Disruptive Technology Initiative
- / DTI Tech Tips
- / Common Data Elements (CDEs) for Clinical Neuropsychology: Sharing is Caring
Common Data Elements (CDEs) for Clinical Neuropsychology: Sharing is Caring
Authors: Naomi Chaytor, Bob Bilder, Robert Kane
Disclosures: Robert Bilder has received honoraria or consulting fees from Atai Life Sciences, Karuna Therapeutics, the Institute of Digital Media and Child Development, and VeraSci, and receives grant support from the National Institute of Mental Health and National Endowment for the Arts.
“Share your knowledge. It is a way to achieve immortality.” — His Holiness the Dalai Lama
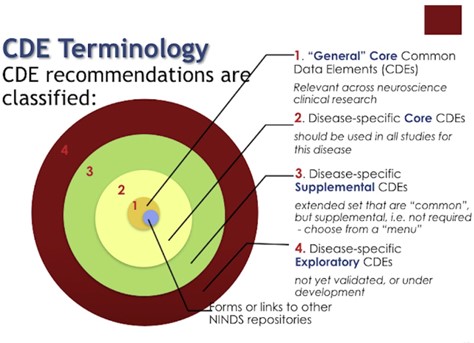
Synopsis: a Common Data Element (CDE) is defined by the National Institutes of Health (NIH) as “a standardized, precisely defined question that is paired with a set of specific allowable responses, that is then used systematically across different sites, studies, or clinical trials to ensure consistent data collection.” CDEs are important to help assure that data can be aggregated across diverse sites, enabling large sample sizes that are necessary to assure robust analyses. In neuropsychological (NP) settings, CDEs include NP test measurements (i.e., test scores), self-report rating scales (e.g., Patient Health Questionnaire or PHQ), interview-based rating scales (e.g., Hamilton Depression Rating Scale), along with demographic and history variables (see below, e.g., REAL and SDOH). CDEs are useful for clinical neuropsychologists because they provide standard assessment formats, enabling data to be combined and thus capable of providing better norms and clinical validation than other scales. CDEs are increasingly used in large electronic medical record systems. For example, standard methods are now being used widely to acquire data on demographic measures like race, ethnicity and language (the “REAL” standards), and on social and structural determinants of health (SDOH). Important standards are emerging to assure appropriate consideration of minoritized groups.
Overall description: CDEs have been advocated by the NIH so that data from different research studies can be pooled (i.e., for “mega-analysis”, which is the joint study of individual case data, as opposed to “meta-analysis” that involves joint study of group data; the individual-level data enables more refined statistical approaches). The NIH has supported several initiatives to advance use of CDEs, including:
- The NIH CDE Repository (https://cde.nlm.nih.gov/home) contains many examples, shows how multiple CDEs (from one or more Collections) can be curated into Forms. Forms in the Repository might be original, or might recreate the format of real-world data collection instruments or case report forms. NIH has endorsed collections of CDEs that meet established criteria. NIH-endorsed CDEs are designated with a gold ribbon.
- The PhenX Toolkit (Phenotypes & Genotypes PhenX Toolkit) supported by the National Human Genome Research Institute), provides a web-based catalog of recommended measurement protocols.
- The National Neuropsychology Network created the Structured History Protocol for Neuropsychology (SHiP-NP) to collect CDEs for demographics, handedness, language proficiency, race, ethnicity, neuropsychological symptoms, and a series of psychiatric symptoms based on the DSM-5 Level 1 Cross-Cutting Assessment, which branches to Level 2 assessments (Psychiatry.org – Online Assessment Measures), and the NINDS CDEs, including the NeuroQoL (quality of life measures), and special CDEs specifically for traumatic brain injury (TBI CDEs). Most CDEs are freely available and there is much published (validity) literature, so these can sometimes replace other costly measures without compromising validity (e.g., compare PROMIS measures of Depression and Anxiety with other proprietary scales).
- There is hope that further work can help establish globally relevant CDEs. Several efforts are underway to advance the goal of international CDEs (see International Alliance of Mental Health Research Funders project “Driving the Adoption of Common Measures”; also the International Neuropsychological Society’s Worldwide Initiative for Neuropsychological Data Sharing.
Case Study Example: The web-based SHiP-NP can be completed by patients, and the provider can then receive an automatically formatted narrative report or tabular output summarizing all the relevant data collected, and these can be pasted into your work processor or electronic medical record; the data can also be saved to your own online databases, and compared to data in the NIMH Data Archive. See also the Harte-Hargrove et al 2018 paper (link below) for an example in epilepsy research, and Loring et al 2022 for further examples.
Helpful links to further reading/material and references:
Harte‐Hargrove, L. C., Galanopoulou, A. S., French, J. A., Pitkänen, A., Whittemore, V., & Scharfman, H. E. (2018). Common data elements (CDEs) for preclinical epilepsy research: Introduction to CDEs and description of core CDEs. A TASK3 report of the ILAE/AES joint translational task force. Epilepsia Open, 3, 13-23.
Loring, D. W., Bauer, R. M., Cavanagh, L., Drane, D. L., Enriquez, K. D., Reise, S. P., … & NNN Study Group. (2022). Rationale and design of the National Neuropsychology Network. Journal of the International Neuropsychological Society, 28(1), 1-11.
Comments/Experiences to Share?
Dear AACN members, please log in to share your comments or questions here.